Ozark Regional Vein & Artery Center helps patients throughout Northwest Arkansas (NWA), Missouri, Oklahoma, Texas, Louisiana, Mississippi, and around the nation. Many of our patients have venous and arterial issues associated with diabetes, including diabetic leg ulcers.
These chronic foot wounds and leg ulcers are an issue in and of themselves. They can lead to much worse situations—possibly life-threatening.
Contact us for treatment for diabetic leg ulcers in NWA, and therapies that can address chronic foot wounds. Plus, we have ways to possibly address the underlying issues that cause them. Our team of medical professionals are ready to provide compassionate care that achieves excellent results.
To begin the healing journey, the first step involves understanding diabetic leg ulcers.
What are diabetic leg ulcers?
Diabetes already affects the body’s ability to break down the food you eat and turn that food into energy. It also causes venous diseases and neuropathic issues, and these can lead to the creation of lesions and ulcers—especially on a sufferer’s legs.
Symptoms of Diabetic Leg Ulcers
How do you know if your diabetes has led to an ulcer or lesion? Certain symptoms point toward the possibility.
- Swelling. Your legs/feet are chronically swollen.
- Drainage. You see blood or pus on your socks or in your shoes.
- Calluses. Your heels are cracked with excessive calluses.
- Blistering. You discover blisters on your swollen legs or feet.
- Open Sores. You have open sores or lesions that aren’t healing well (or at all).
- Wounds. You find wounds on your legs/feet that you don’t remember getting.
- White spot. If your skin has a whitish spot, it could be a sign of poor/lost circulation.
What does the ulcer look like when it starts?
In most cases we’ve seen at our clinic in northwest Arkansas, the ulcer starts as an open sore or wound on the lower leg, ankle, bottom of the foot or on the toes. This sore could have been caused by a scratch, a splinter maybe, or even a blister that went unnoticed because of the neuropathy associated with many cases of diabetes.
This wound can look like any other scratch, abrasion, puncture, or blister. However, it becomes an ulcer when it doesn’t heal. These ulcerations can become extremely painful, as it remains an open wound that can come in contact with clothing, or become infected if not properly treated.
If you suffer from diabetes and have swollen or numb legs, be sure to have any injury you find looked at by your health provider as soon as possible. Your first avenue to getting better? Helping your body help itself heal through treatment for diabetic leg ulcers in NWA.
Levels of diabetic foot ulcers
Diabetic ulcers found on your feet are usually graded for treatment using their size, their depth, and the area they affect. The grade usually falls into 1 of the 6 following levels.
Level 1
Your foot is generally normal with no apparent signs of ulceration. Most often healthcare providers will recommend you care for your feet with greater attention, and make sure your shoes fit well without undue points of pressure or contact.
Level 2
You may exhibit evidence of neural damage (numbness, tingling) or reduced circulation (whitish skin, spider veins, varicose veins). This heightens the risk of foot/leg ulcers. Also, calluses and/or corns on your feet can cause unnecessary pressure points, so your provider may remove the dead skin through debridement.
Level 3
At the 3rd level, an ulcer has formed. Your doctor may want you to decrease the pressure that you put on the ulcerated foot/leg. This may require anything from an air-cushioned walking brace (an “Aircast”) to ambulatory use of a wheelchair to prescribed bed rest.
Level 4
At this level the ulcer has become infected. Your provider will test the infection using a culture to identify the cause. Depending on the source and extent of the infection, antibiotics may be prescribed, or surgery may be required to remove infected tissue.
Level 5
This progression exhibits dead tissue, caused either by the infection or insufficient circulation. Usually considered to be gangrene, this level involves a hospital stay and intravenous antibiotics. If the gangrene is more advanced, surgery may be required to cut away the dead tissue.
Control of the infection and gangrene remediation are imperative, as the depth of the infection could reach bone, or enter the bloodstream (sepsis).
Which gangrene is most common with Level 5 diabetic leg ulcers?
As a diabetes sufferer, your biggest risk is developing “dry gangrene.” This occurs when blood flow is blocked and the tissue dies.
The second most common gangrene is “wet gangrene.” This tissue death occurs as a combination of the injury (scratch, puncture, etc), the ensuing bacterial infection, and the lack of circulation to get infection-fighting blood flow at the injury site. The sore/ulcer exhibits leakage and a “wet” infection site.
That lack of circulation inhibits your immune system’s ability to fight infection and repair damaged tissue. That’s why it’s so important to work with a vascular care specialist like here at Ozark Regional Vein & Artery center, so that you have treatment for diabetic leg ulcers in NWA, and professional treatment choices for gangrene.
Level 6
This level exhibits damage that’s so severe, and gangrene that’s so prevalent, that the foot (or leg) must be removed. Even after this surgery, special care must be taken to not cause pressure ulcers to form on the remaining leg/foot. Therapeutic sleep devices will probably be recommended to help alleviate pressures.
Types of Ulcers
There are 3 types of ulcers that appear most frequently on a diabetic’s legs and feet.
Neuropathic
If diabetes has caused nerve damage and limited or lost feeling, sensory/peripheral neuropathy occurs. In this condition, the patient doesn’t feel trauma or injury to the skin, or at best has a constant “pins and needles” feeling, akin to when a body part “falls asleep” because of restricted blood supply.
When your nervous system doesn’t register that leg or foot injury (sensation of pain), the wound can go unknown and untreated. This leads to infection and the creation of a chronic foot or leg ulcer.
Ischaemic
An ischaemic leg or foot wound can ulcerate because type 1 or type 2 diabetes has caused peripheral arterial disease (PAD). This disease causes poor circulation due to multiple issue presentations in the veins and arteries.
This poor blood supply and obstructed circulation, along with the bloating caused by the pooling of blood in the legs, means that wounds don’t heal well, or sometimes at all.
Ischaemic ulcers have a higher risk of severe issues because of the possible chronic wounds. If these wounds can lead to deeper/worsened infections, tissue death (gangrene), and amputation.
If the infection enters the bloodstream, it can lead to sepsis. This extremely serious situation can cause organ damage, or even cause death.
NeuroIschaemic
Neuroischaemic ulcers combine the worst of two worlds. The patient doesn’t feel these chronic foot wounds (neuropathy), nor does their inadequate blood supply allow proper healing (ischemia). Neuroischaemic issues and their causative factors lead to higher rates of amputation and/or mortality.
Diabetic Ulcers vs Venous Stasis Ulcers
What is the difference between venous stasis ulcer and diabetic ulcer? It’s delineated by the root cause of the venous issue.
Venous stasis and any ensuant ulcers aren’t necessarily caused by diabetes. Venous stasis happens when the valves in a patient’s veins are damaged. Because these valves control the blood pressure in the veins, it can cause swelling in the extremities—especially when walking.
The leg swelling can be extreme, with the worst effects occurring in the lower legs, ankles, and feet. This swelling can put enough pressure on skin to cause an ulcer to form, usually on/around the ankles. The ulcers acn form because of other leg vein issues, such as varicose veins and/or chronic venous insufficiency.
Unlike neuropathic ulcers, these wounds can be felt, often presenting as an achy or dull pain throughout the leg. Because sufferers are at least aware there’s an issue, treatment can be performed.
Venous stasis ulcers usually heal in 3 to 4 months. You should consult with a healthcare professional to ensure proper diagnosis and treatment. Contact us at Ozark Regional Vein & Artery Center for help healing, and to understand how to best prevent further issues.
FAQs
Can diabetic leg ulcers be cured?
Yes, these ulcers can be treated and even cured, depending on the level of the wound and on the severity of the ischaemic issues. The lower extremity arterial disease doesn’t necessarily stop healing, but it can greatly slow it down. Getting the wound to heal will require daily wound care, and patience. It may take weeks or even months for treatment for diabetic leg ulcers in NWA to finish the healing.
What are diabetic foot ulcers?
This type of skin lesion involves an open sore on your foot, frequently on the bottom of the foot (where the most pressure is exerted when walking). About 1 in 20 diabetes patients develop foot ulcers. Of those, approximately 60% also have neuropathy.
These foot ulcers are the most common reason for hospital admission when compared to other diabetic complications. Though a chronic condition, it’s often preventable with heightened foot care and regular health provider visits.
Who gets diabetic foot ulcers in northwest Arkansas?
Any patient with diabetes can develop a foot ulcer. They occur more frequently in patients who are 45 years old or older. Latinos, African Americans, and Native Americans incur higher rates of diabetic foot ulcers in the United States.
How does a diabetic ulcer form?
For diabetics, neuropathy contributes the most to the formation of diabetic leg ulcers. The lack of feeling means wounds and other issues (corns, calluses) can happen without the patient feeling the warning signs (pain). When ischaemic issues are also present, the circulatory deficiency compounds the situation, making it easier for a sore or wound to become an ulcer. If you think you’re having issues, come in for treatment for diabetic leg ulcers in NWA so that you can get better, faster.
Finding Treatment for Diabetic Leg Ulcers in NWA
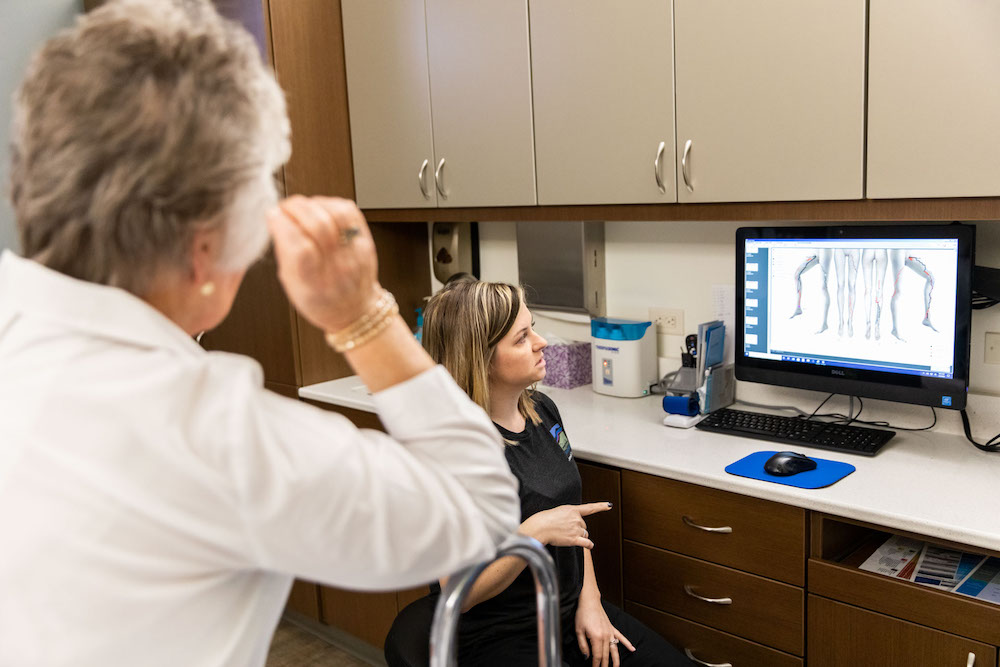
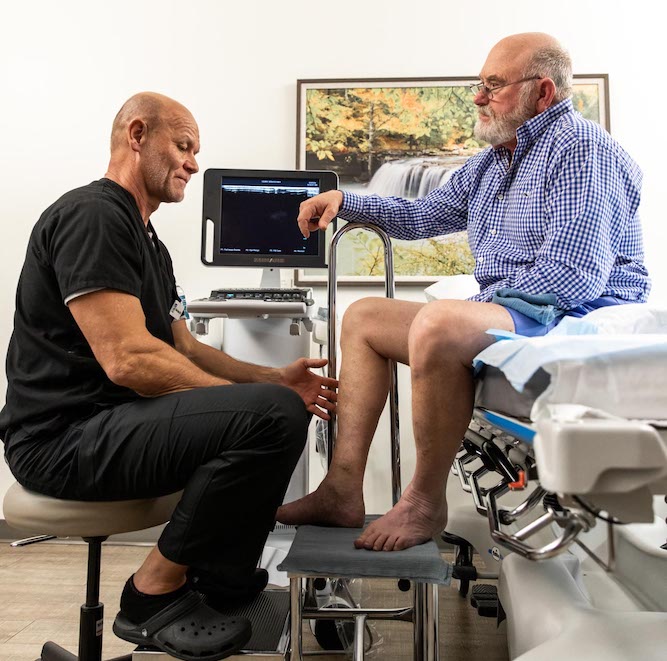
At Ozark Regional Vein & Artery Center, Dr. Stout is uniquely qualified to perform any type of vascular procedure outside of the heart, including the treatment of leg ulcers.
Arterial disease and the effects of diabetes can progress to the point where ulcers appear on the legs or feet, and immediate action must be taken to improve circulation so that your body can fight infection and heal the wound.
Dr. Stout is Certified by The American Board of Surgery in Vascular and General Surgery. He holds memberships in the Society for Vascular Surgery and Society for Vascular Ultrasound. Along with being a published author for vascular care, Dr. Stout is a public speaker, having addressed international vascular meetings in addition to regional and national vascular meetings.
Take the first step to recovery with our Virtual Vascular Screening Tool. We also hold regular free screening events and invite you to join us for education with compassion and answers with heart. We listen, we care, and we commit.
Contact us today with your questions about diabetic leg ulcers, and any other vein or artery issues—or schedule a consultation. We offer cutting-edge treatments, concierge-level care, and a professional medical team dedicated to your health.