Diabetes is one of the single most common health conditions on the planet, with nearly 21 million cases in the United States alone. Patients contending with diabetes deal with a host of health complications, most of which can severely decrease the quality of a patient’s life. As a vascular care center, however, we’re interested in tackling a major question we receive from our patients: how does diabetes damage blood vessels?
That question can be tricky to explore in its totality. Diabetes is an incredibly complex, and interconnective health concern, and the last thing we want to do is confuse patients with a bunch of medical jargon that doesn’t mean anything to them. Nor do we want to scare you with frightening statistics or possible health outcomes. We want to educate you and help you make informed healthcare decisions. Your safety and well-being are our priority.
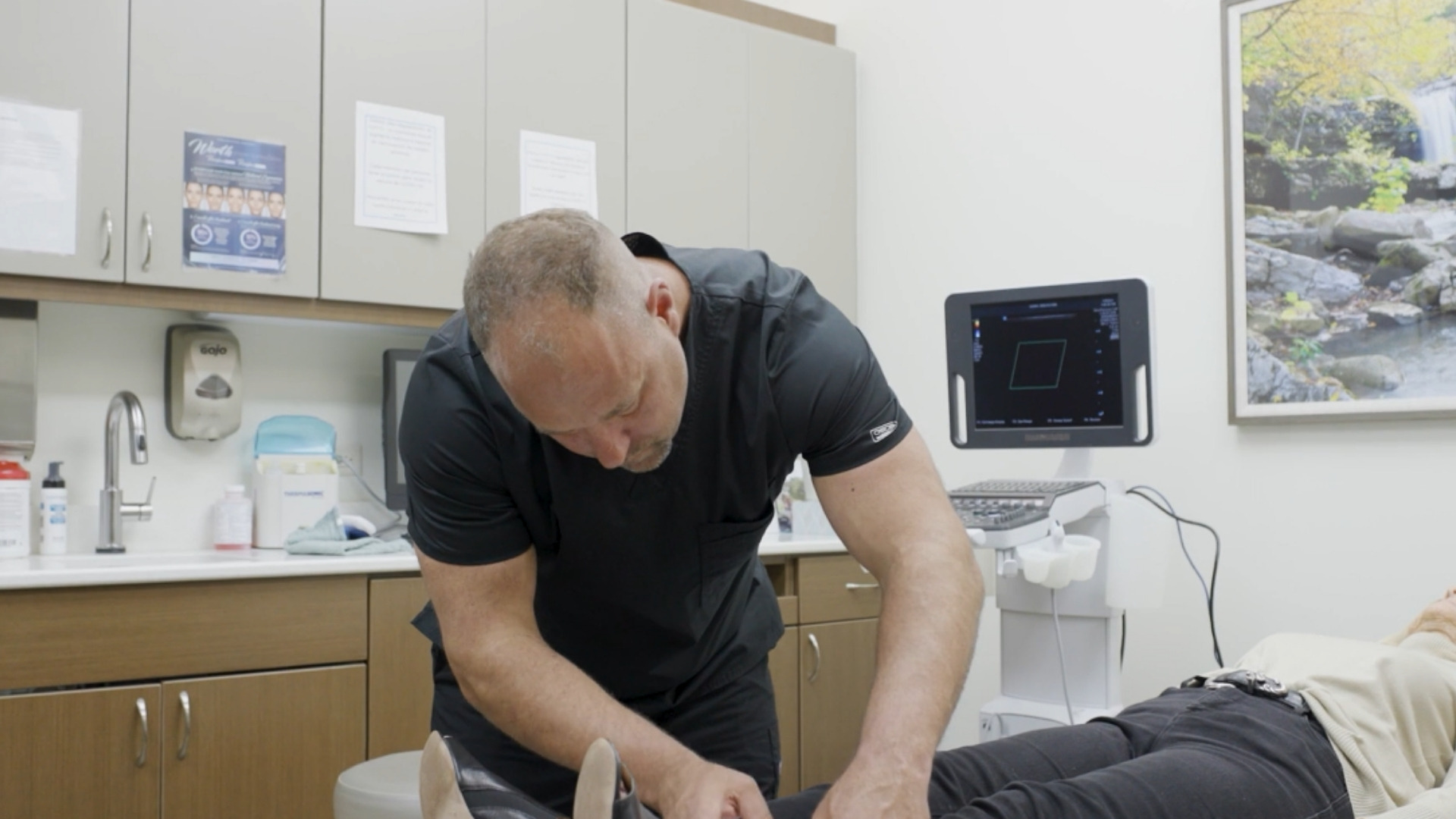
But, given how many patients dealing with arterial disease and vascular concerns are also juggling care strategies for diabetes, we decided it was time to tackle the issue. As a result, the Ozark Regional Vein & Artery Center turned to our resident vascular surgeon, Dr. Christopher Stout, for a breakdown of all things Diabetes.
What does the condition entail? How does diabetes damage blood vessels? What is the science behind that progression? Are there known complications? What causes Diabetes? Most importantly of all: What are the treatment options and preventative measures available for patients dealing with curable diabetes varieties?
Here’s everything you could ever want to know about Diabetes, Arterial Disease, and the cost of living with both.
Diabetes 101
Diabetes is a disease in which the body does not produce or properly use insulin. Insulin is a hormone needed to convert sugar, starches, and other food into energy needed for daily life.
Glucose—a sugar—is the main energy source for the cells that make up muscles and other body tissues. Insulin is vital for breaking down glucose within our bloodstream to allow tissue to absorb it as energy. This process of breaking down sugars into absorbable chemicals is how we fuel our bodies.
Additionally, this process requires our bodies to be incredibly efficient at regulating the level of glucose in our bloodstream. When glucose levels are low, such as when you haven’t eaten in a while, the liver breaks down stored glycogen—excess glucose kept in the liver—into glucose. This keeps our bodies regularly fueled and operating at peak efficiency. It also, critically, keeps glucose levels within a typical range.
For patients with diabetes, however, there’s either no insulin (type 1) to let glucose into the cells, or so much glucose (type 2) that an excess of insulin is necessary to accomplish systemic stability. Because of this, sugar builds up in the bloodstream. This can cause life-threatening complications.
Over time, diabetes complications can affect major organs in the body. These organs include the heart, blood vessels, nerves, eyes, and kidneys. Having a normal blood sugar level can lower the risk of many complications.
Types of Diabetes
There are 4 commonly recognized varieties of diabetes. These include:
Type 1
Type 1 diabetes is an autoimmune disorder in which the body’s immune system destroys insulin-producing beta cells. As a result, the body cannot produce insulin, the hormone that breaks down glucose, allowing it to enter and fuel the cells. To survive, individuals with type 1 diabetes must take insulin every day. It is estimated that 5-10% of all diabetes cases diagnosed nationwide are type 1 diabetes.
Type 2
Type 2 diabetes is the most common type of diabetes, accounting for 90-95% of all diabetes. In type 2 diabetes, the body does not produce enough insulin and/or the body’s cells become resistant to insulin. This results in a condition called insulin resistance.
Gestational
Gestational diabetes occurs in some women who have extremely elevated blood glucose levels during pregnancy but have never had diabetes. Between 4-8% of pregnant women experience gestational diabetes, but it isn’t always clear what causes the condition. One possibility is that hormones released into the body to help with pregnancy—and keeping a gestating fetus healthy—can sometimes block the action of the mother’s insulin in her body.
This insulin resistance makes it hard for the mother’s body to use insulin to break down glucose. And this means that she may need up to three times as much insulin than normal to compensate.
Gestational diabetes can also start when the mother’s body is not able to make and use all the insulin it needs for pregnancy. Without enough insulin, glucose can’t leave the blood and be changed into energy. When glucose builds up in the blood, it’s called hyperglycemia.
Prediabetes
Prediabetes is a condition that occurs when a person’s blood glucose levels are higher than normal but not high enough for a diagnosis of type 2 diabetes. It is estimated that there are approximately 41 million Americans who have prediabetes, in addition to the 20.8 million Americans currently living with diabetes.
The Connection Between Diabetes and Vascular Disease
If you do not manage your diabetes or maintain healthy habits, you could develop serious health conditions, including blindness, severe kidney disease, stroke, heart attack, sores in your feet, or gangrene (dead tissue) that could lead to infection and eventually to amputation.
Diabetes is linked to several vascular diseases:
- Retinopathy, an abnormal growth of blood vessels in your retina
- Nephropathy, a disease that damages the tiny filtering units of the kidney
- Neuropathy, a condition causing a loss of sensation in the feet and toes
- Atherosclerosis
- Stroke
- Peripheral Artery Disease (PAD)
How Does Diabetes Damage Blood Vessels?
So, speaking very explicitly, how does Diabetes damage blood vessels? Well, they do it by exacerbating arterial disease.
People with diabetes are at much greater risk for heart and vascular disease compared to people who do not have diabetes.
Conditions associated with diabetic arterial disease include:
- Heart attacks
- Strokes
- Non-healing wounds in the legs and feet
- High blood pressure
Causes of diabetic arterial disease
People with diabetes have too much sugar in their blood. This may change blood chemistry and cause blood vessels to narrow. In some cases, it can damage blood vessels—a process known as atherosclerosis.
Atherosclerosis is the first stage of all other arterial diseases. As plaque builds up within an artery, it leads to the progressive thickening of the artery’s lining. This thickening process slowly narrows the artery’s interior, a process best described as hardening of the arteries.
If enough plaque builds up to narrow or block an artery for a prolonged period, it can cause damage to tissue and organs. The health problems that result depend on the location of any narrowing or blockage. All other vascular diseases stem from plaque buildup and arterial hardening.
Diabetic arterial disease risks
Factors that can increase your risk for diabetic vascular disease include:
- How long you have had diabetes
- How well you control your diabetes
- High blood pressure or high cholesterol levels
- Tobacco use
- An inactive lifestyle
- If you are overweight or obese
- A high-fat diet
These factors can also worsen diabetic arterial disease that already exists.
Diabetic arterial disease complications
People with diabetes are more likely to have a heart attack, stroke, or experience kidney disease.
Diabetic arterial disease typically affects smaller arteries—including those that lead to the eyes, kidneys, fingers, feet, and toes—causing nerve and circulation problems. This combination can create several health issues, such as loss of feeling in the feet.
Because many people with diabetes develop nerve problems, they may not notice that their feet are injured, which can lead to:
- Sores (ulcers) that heal slowly or do not heal
- Infection
- Tissue death (gangrene), in the worst cases, which can lead to amputation
The Science of How Diabetes Impacts Arterial Disease
The major point of this blog is to answer that all-important question: how does diabetes damage blood vessels? After all, as a vein and artery clinic, educating patients on their vascular health is our primary goal.
People with diabetes are at higher risk of developing atherosclerosis, the most common cause of peripheral artery disease (PAD). And people with PAD have a much higher risk of heart attack or stroke.
PAD is similar to coronary artery disease (blockage in arteries that supply blood to the heart muscle) and carotid artery disease (blockage in arteries leading to the brain). However, with PAD, the arteries lead to areas outside the brain and heart that become blocked, including the neck, arms, and belly, but most often in the legs and feet (lower-extremity PAD).
Fatty deposits build up in the inner linings of the artery walls of the legs, making them narrower, hindering blood flow, and can even stop blood flow to the legs and feet. This condition can lead to pain, especially when walking. Other symptoms include foot wounds that are slow to heal, one foot being much colder than the other, or gangrene. In severe cases, patients may need foot or leg amputation.
Learn more about the Ins & Outs of Arterial Disease Care in Rogers→
Diabetes Complications
Vascular diseases, particularly atherosclerosis, are major causes of disability and death in patients with diabetes. Diabetes substantially increases the risk of developing coronary, cerebrovascular, and peripheral arterial disease. The pathophysiology of vascular disease in diabetes involves abnormalities in blood flow, blood composition, and glucose absorption by organs and cells throughout the body.
This can result in:
- Nerve damage (neuropathy). Too much sugar in the blood can injure the walls of the tiny blood vessels (capillaries) that feed the nerves. This is especially true in the legs. This can cause tingling, numbness, burning or pain. This usually begins at the tips of the toes or fingers and spreads upward. Poorly controlled blood sugar could cause you to lose all sense of feeling in the affected limbs over time.
- Kidney damage (nephropathy). The kidneys have millions of tiny blood vessels that keep waste from entering the blood. Diabetes can damage this system. Severe damage can lead to kidney failure or end-stage kidney disease that can’t be reversed. End-stage kidney disease needs to be treated with mechanical filtering of the kidneys (dialysis) or a kidney transplant.
- Eye damage (retinopathy). Diabetes can damage the blood vessels in the retina, the light-sensing part of the eye.. This could cause blindness. Diabetes also increases the risk of other serious vision conditions, such as cataracts and glaucoma.
Amputation
“How does diabetes damage blood vessels?” shouldn’t be the only question you ask, though it is an important one. Another question to ask is, “does diabetes increase my likelihood of amputation?” The admittedly scary answer is yes.
These abnormalities also contribute to health complications like nerve damage and poor blood circulation in the limbs. These problems make the feet vulnerable to skin sores (ulcers) that can worsen quickly.
These ulcers—open sores on the body—can be slow-healing and prone to infection. In some severe cases, ulcers can even lead to gangrene or claudication. As a result, many patients that require amputation or limb salvage support usually are dealing with physical complications from arterial disease and diabetes.
The good news is that proper diabetes management and careful foot care can help prevent foot ulcers.
Partnering with a Vascular Surgeon for Amputation Prevention in Rogers→
Higher Risk for Foot Ulcers
When foot ulcers do develop, it’s essential to get prompt care. A nonhealing ulcer that causes severe damage to tissues and bone may require surgical removal (amputation) of a toe, foot, or part of a leg. More than 80 percent of amputations begin with foot ulcers.
Some people with diabetes are more at risk than others. Factors that lead to an increased risk of amputation include:
- High blood sugar levels
- Smoking
- Nerve damage in the feet (peripheral neuropathy)
- Calluses or corns
- Foot deformities
- Poor blood circulation to the extremities (peripheral artery disease)
- A history of foot ulcers
- A past amputation
- Vision impairment
- Kidney disease
- High blood pressure
Here’s what you need to know to start your at-home foot health routine, including key signs that it’s time to see a doctor.
Preventing foot ulcers
Proper foot care will help prevent problems with your feet and ensure you know to seek out care if issues do start to appear. This includes:
- Inspect your feet daily. Check your feet daily for blisters, cuts, cracks, sores, redness, tenderness, or swelling. If you have trouble reaching your feet, use a hand mirror to see the bottoms of your feet.
- Clean your feet. Wash your feet in lukewarm (not hot) water once a day. Dry them gently, especially between the toes. Use a pumice stone to gently rub the skin where calluses easily form. You should also sprinkle talcum powder or cornstarch between your toes to keep the skin dry. Use a moisturizing cream or lotion on the tops and bottoms of your feet to keep the skin soft.
- Don’t remove calluses or other foot lesions yourself. To avoid injury to your skin, don’t use a nail file, nail clipper, or scissors on any calluses, corns, bunions, or warts. Don’t use chemical wart removers. See your doctor or foot specialist to remove any of these lesions.
- Don’t go barefoot. Don’t go barefoot, even around the house, to prevent injury to your feet.
- Buy shoes that fit properly. Buy comfortable, or orthopedic, shoes that provide support and cushioning for the foot’s heel, arch, and ball. Avoid tight-fitting shoes and high heels or narrow shoes that crowd your toes. If one foot is bigger than the other, buy shoes in the larger size.
We also encourage you to wear clean, dry socks. This helps keep your feet clean and protected.
- Schedule regular foot checkups. Your doctor can inspect your feet for early signs of nerve damage, poor circulation, or other foot problems. Schedule foot exams at least once a year or more if your doctor recommends them.
Signs of trouble
Contact your doctor if you have:
- Ingrown toenails
- Blisters
- Plantar warts on the soles of your feet
- Athlete’s foot
- An open sore or bleeding
- Swelling
- Redness
- Warmth in one area
- Pain (though you may not feel anything if you have nerve damage)
- Discolored skin
- A foul odor
- An ulcer that lasts longer than one to two weeks
- An ulcer bigger than 3/4 inch (2 centimeters)
- A sore that doesn’t quickly begin to heal
- An ulcer so deep you can see the bone underneath
Your doctor will inspect your foot to make a diagnosis and prescribe the appropriate course of treatment.
Causes
Diabetes causes vascular disease if there is too much glucose in the blood. This excess glucose damages the blood vessels.
The exact cause of type 1 diabetes is currently not understood by science. Our best understanding is that the body’s own immune system—which normally fights harmful bacteria and viruses—misidentifies and then targets the insulin-producing cells in the pancreas, thereby destroying them. There is also, however, some belief among doctors that there may be a hereditary link to the spread of the condition, and uncertainty surrounding the condition as a response to viruses and/or environmental exposure early in life.
Though the uncertainty of what causes type 1 diabetes can prove incredibly frustrating to patients, the fact it usually appears so early in life makes it easier to monitor. With proper treatment, many people with type 1 diabetes live incredibly normal, comfortable lives.
Type 2 diabetes is associated with older age, obesity, physical inactivity, a family history of diabetes, a history of gestational diabetes, and race and ethnicity. Specifically, studies show that as a result of a variety of genetic and social factors, racial and ethnic minorities have a far higher prevalence of type 2 diabetes than the population at large.
Warning Signs
Some symptoms of diabetes include:
- Frequent urination
- Excessive thirst
- Extreme hunger
- Unusual weight loss
- Increased fatigue
- Irritability
- Blurry vision
Some symptoms of diabetes-related vascular problems include:
- Blurred vision
- Floating spots in your vision
- Unexpected weight gain or swelling in your face or limbs
- Foamy looking urine
- Sores on your feet
- Loss of feeling in your hands or feet
- Burning feeling in your hands or feet
- Pain in your legs when walking
- High blood pressure
- Chest pain
Treatment & Prevention
The best strategy for preventing complications of diabetes is proper diabetes management with a healthy diet, regular exercise, blood sugar monitoring, and adherence to any necessary, prescribed medication regimen.
You should talk to your primary care provider if you’re interested in learning more!
Conservative Care
If you’re looking for more specific steps you can take to improve your artery health, here are a few activities you can do to improve arterial health and overall circulation:
Avoid Smoking.
Smoking is one of the worst things you can do for your vascular system, so our first piece of advice is to stop smoking immediately. Smoking contributes to the buildup of plaque in the arteries, meaning it’s a major risk factor for the development of arterial disease and a decrease in quality of life.
Exercise.
Exercising is a great way to improve vascular health, as it keeps blood flowing and prevents further plaque buildup. Walking and cardiovascular exercise are incredibly beneficial, but anything that elevates your heart rate is good. You should make a point of exercising once a day or as much as is feasible.
Eat Healthier.
Diet is a major contributing factor to arterial disease. Foods high in cholesterol are a major cause of plaque buildup and increased blood pressure. One way to avoid this outcome is to eat more fruits and vegetables and less red meat and dairy. You should also make sure to eat smaller portions in individual sittings to reduce stress on your circulatory system.
Lose Weight.
This item is the most difficult. Being overweight can significantly strain your circulatory system, as it requires more work to move blood around your body. Losing weight is vital to improving circulatory function and overall vascular health.
Monitor Your Health.
Make sure to check your blood pressure and cholesterol levels regularly to keep tabs on your arterial health! Routine health screenings and physicals are critical to maintaining your overall physical health and can be especially useful for identifying and mitigating arterial disease.
Note: It’s important to remember that none of these behaviors should replace consulting a healthcare provider or vascular specialist if you are worried about your vascular health.
Turn to the Ozark Regional Vein & Artery Center
Now that you know the answer to, “how does diabetes damage blood vessels?” you have some decisions to make.
If you require support treating arterial disease complicated by diabetes or are looking to tackle diabetic arterial disease, come to the Ozark Regional Vein & Artery Center. Our experience and growing suite of care options enable us to guide you toward lasting wellness solutions for a happier, healthier life.
We are the premier practice in Northwest Arkansas for all the highest-quality vein treatments available. Patients come to Dr. Haney, Dr. Stout, and the expert staff from all over Northernwestern Arkansas, from Fayetteville to Bentonville, to ensure they receive the best concierge-level care and leg vein procedures.
After all, helping people is what we do, and our mission is to provide the people of Northwestern Arkansas and beyond with the absolute best care possible. Our ever-expanding areas of expertise and commitment to patient education help us achieve meaningful results for our patients every time.
Lead the charge on your vascular care with our Virtual Vein Screening Tool or by scheduling a consultation.